|
BOOK NOW |
ASK ABOUT YOUR PAIN |
Home > Blog > Physiotherapy & Hand Therapy > Tendinopathy Physiotherapy
Tendinopathy Physiotherapy
Tendinopathy, also known as tendinitis or tendinosis, is a type of tendon disorder that results in pain, swelling, and impaired function. The pain is typically worse with movement.
It most commonly occurs around the
- shoulder (rotator cuff tendinitis, biceps tendinitis)
- elbow (tennis elbow, golfer's elbow)
- wrist
- hip
- knee (jumper's knee)
- ankle (Achilles tendinitis)
Causes may include an injury or repetitive activities.
Groups at risk include people who do manual labor, musicians, and athletes. Less common causes include infection, arthritis, gout, thyroid disease, and diabetes.
Diagnosis is typically based on
- symptoms
- examination
- occasionally medical imaging
A few weeks following an injury little inflammation remains, with the underlying problem related to weak or disrupted tendon fibrils.
Treatment may include rest, NSAIDs, splinting, and physiotherapy.
Less commonly steroid injections or surgery may be done. About 80% of people get better within 6 months. Tendinopathy is relatively common. Older people are more commonly affected. It results in a large amount of missed work (ergonomics and productivity matters)
Signs and symptoms
Symptoms includes tenderness on palpation and pain, often when exercising or with movement.
Cause
Causes may include an injury or repetitive activities such as tennis. Groups at risk include people who do manual labor, musicians, and athletes. Less common causes include infection, arthritis, gout, thyroid disease, and diabetes.
Despite the injury of the tendon there is poor healing.
Quinolone antibiotics are associated with increased risk of tendinitis and tendon rupture. A 2013 review found the incidence of tendon injury among those taking fluoroquinolones to be between 0.08 and 0.2%. Fluoroquinolones most frequently affect large load-bearing tendons in the lower limb, especially the Achilles tendon which ruptures in approximately 30 to 40% of cases.
Types
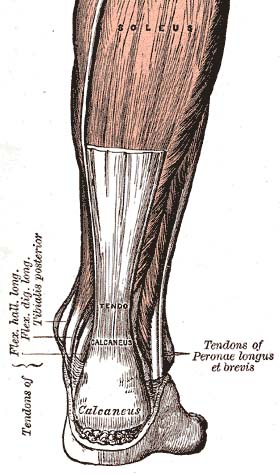
- Achilles tendinitis
- Calcific tendinitis
- Patellar tendinitis (jumper's knee)
Pathophysiology
As of 2016 the pathophysiology is poorly understood; while inflammation appears to play a role, the relationships among changes to the structure of tissue, the function of tendons, and pain are not understood and there are several competing models, none of which had been fully validated or falsified.
Molecular mechanisms involved in inflammation includes release of inflammatory cytokines like IL-1β which reduces the expression of type I collagen mRNA in human tenocytes and causes extracellular matrix degradation in tendon.
There are multifactorial theories that could include: tensile overload, tenocyte related collagen synthesis disruption, load-induced ischemia, neural sprouting, thermal damage, and adaptive compressive responses.
The intratendinous sliding motion of fascicles and shear force at interfaces of fascicles could be an important mechanical factor for the development of tendinopathy and predispose tendons to rupture. Obesity, or more specifically, adiposity or fatness, has also been linked to an increasing incidence of tendinopathy.
The most commonly accepted cause for this condition however is seen to be an overuse syndrome in combination with intrinsic and extrinsic factors leading to what may be seen as a progressive interference or the failing of the innate healing response.
Tendinopathy involves
- cellular apoptosis
- matrix disorganization
- neovascularization
Classic characteristics of "tendinosis" include degenerative changes in the collagenous matrix, hypercellularity, hypervascularity, and a lack of inflammatory cells which has challenged the original misnomer "tendinitis".
Histological findings include granulation tissue, microrupture, degenerative changes, and there is no traditional inflammation. As a consequence, “lateral elbow tendinopathy or tendinosis” is used instead of “lateral epicondylitis”.
Examination of tennis elbow tissue reveals noninflammatory tissue, so the term “angiofibroblastic tendinosis” is used.
Cultures from tendinopathic tendons contain an increased production of type III collagen.
Longitudinal sonogram of the lateral elbow displays thickening and heterogeneity of the common extensor tendon that is consistent with tendinosis, as the ultrasound reveals calcifications, intrasubstance tears, and marked irregularity of the lateral epicondyle.
Although the term “epicondylitis” is frequently used to describe this disorder, most histopathologic findings of studies have displayed no evidence of an acute, or a chronic inflammatory process.
Histologic studies have demonstrated that this condition is the result of tendon degeneration, which causes normal tissue to be replaced by a disorganized arrangement of collagen. Therefore, the disorder is more appropriately referred to as “tendinosis” or “tendinopathy” rather than “tendinitis.”
Colour Doppler ultrasound reveals structural tendon changes, with vascularity and hypo-echoic areas that correspond to the areas of pain in the extensor origin.
Load-induced non-rupture tendinopathy in humans is associated with an increase in the ratio of collagen III:I proteins, a shift from large to small diameter collagen fibrils, buckling of the collagen fascicles in the tendon extracellular matrix, and buckling of the tenocyte cells and their nuclei.
Diagnosis

Symptoms can vary from aches or pains and local joint stiffness, to a burning that surrounds the whole joint around the inflamed tendon. In some cases, swelling occurs along with heat and redness, and there may be visible knots surrounding the joint.
With this condition, the pain is usually worse during and after activity, and the tendon and joint area can become stiff the following day as muscles tighten from the movement of the tendon. Many patients report stressful situations in their life in correlation with the beginnings of pain which may contribute to the symptoms.
Medical imaging
Ultrasound imaging can be used to evaluate tissue strain, as well as other mechanical properties.
Ultrasound-based techniques are becoming more popular because of its affordability, safety, and speed. Ultrasound can be used for imaging tissues, and the sound waves can also provide information about the mechanical state of the tissue.
Tendinopathy Physiotherapy
Following diagnosis, our senior physiotherapist will then create a custom physio intervention plan for you, and depending on the causes of the problem, you may be treated with a combination
- heat therapy to loosen the muscles, tissues and joints
- cold therapy to decrease inflammation and pain
- ultrasound therapy to accelerate soft tissue healing
- manual therapy
- joint manipulation and mobilization to increase the natural range
- pain relief physiotherapy
- stretching and flexibility physiotherapy
- dry needling physiotherapy
- computerized decompressive spinal traction
- strengthening exercises
- core stability strengthening